Antibiotics Shouldn't Be Used Recklessly: Are You Still Falling for These Common Misconceptions?
Antibiotics are undoubtedly one of the "star medications" in modern medicine, saving countless lives by helping us fight bacterial infections like pneumonia, urinary tract infections, and tonsillitis. However, while antibiotics are life-saving, they are not a cure-all. Misusing or overusing them can lead to serious health problems. So how should antibiotics be used correctly? What are the common misconceptions you might still be falling for? Let’s dive into the "little secrets" of antibiotic use.
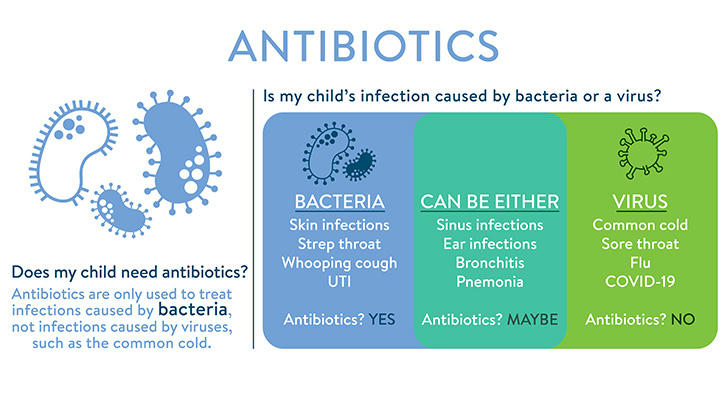
Myth 1: Antibiotics Can Treat All Infections
One of the most widespread misconceptions is that antibiotics can treat any kind of infection. In reality, antibiotics are only effective against bacterial infections and do nothing for viral infections. For example, the common cold, the flu, and a cough are all caused by viruses, and antibiotics have no impact on them.
Take the common cold, for instance. Taking antibiotics won’t help you recover faster. In fact, misusing antibiotics not only won’t improve your condition but could also weaken your immune system, making it less effective at fighting off future bacterial infections. Misuse can even contribute to the development of antibiotic resistance.
Myth 2: You Need Antibiotics When You Have a Cold
Many people believe that antibiotics are a must-have when they catch a cold. However, since colds are caused by viruses, antibiotics are completely ineffective in treating them. The best course of action for a cold is to rest, stay hydrated, and use over-the-counter remedies to alleviate symptoms.
Only if a cold is followed by a bacterial infection, such as pneumonia or bacterial throat infections, would a doctor consider prescribing antibiotics. So, during a cold, you shouldn’t self-prescribe antibiotics but should consult a healthcare professional to determine the appropriate treatment.
Myth 3: Once You Feel Better, You Can Stop Taking Antibiotics
This is a mistake many people make. After a few days of taking antibiotics, they may feel better and assume they’re cured, stopping their medication prematurely. This is dangerous. Antibiotics need to be taken for the full prescribed course, even if you start feeling better. If you stop too soon, the bacteria may not be completely eliminated, and you risk the infection returning, potentially even stronger. Furthermore, stopping antibiotics early can contribute to antibiotic resistance.
For bacterial infections, completing the full course of antibiotics—usually 5 to 7 days—is crucial, even if symptoms improve. This ensures that all the bacteria are eradicated.
Myth 4: Higher Doses of Antibiotics Work Faster and Better
Some people think that increasing the dose of antibiotics will speed up recovery. This is a dangerous misunderstanding. In fact, taking more antibiotics than prescribed can lead to serious side effects, including damage to organs like the liver and kidneys. Overuse of antibiotics also accelerates the development of antibiotic-resistant bacteria.
Antibiotics should always be taken according to a doctor's prescription, with the proper dose and duration, to minimize side effects and prevent the development of resistant bacteria.

Myth 5: All Bacterial Infections Can Be Treated with the Same Antibiotic
Another misconception is that any bacterial infection can be treated with just one type of antibiotic. In reality, different types of bacteria respond to different antibiotics. For example, penicillin may work for certain bacteria but is ineffective against others.
Self-prescribing antibiotics without knowing the specific bacteria involved could make the infection worse. The right approach is to get a doctor's diagnosis and, if necessary, conduct bacterial culture or antibiotic sensitivity testing to choose the most effective antibiotic.
Myth 6: Leftover Antibiotics Can Be Used for Future Illnesses
Many people keep leftover antibiotics and use them the next time they get sick. This is a risky practice. Expired antibiotics may lose their effectiveness, and using the wrong antibiotic for a new infection may make things worse. In addition, different bacterial infections require different treatments, so you cannot assume that the same antibiotic will work for a new illness.
Every time you’re ill, you should see a doctor for a new prescription, rather than relying on leftover medication.

Myth 7: Antibiotics Don’t Have Side Effects
Some people believe that antibiotics are "magic pills" that don't come with side effects. While antibiotics are generally safe, they can cause side effects, especially when misused. Common side effects include gastrointestinal issues (like nausea or diarrhea), allergic reactions, and liver or kidney damage. More seriously, overuse can disrupt your gut bacteria and contribute to the development of superbugs—bacteria that are resistant to multiple antibiotics.
Superbugs are becoming increasingly common, and once they develop, they are much harder to treat. This is why it’s crucial to use antibiotics only when necessary and under medical supervision.
Conclusion: Use Antibiotics Responsibly to Protect Your Health
Antibiotics are an essential tool in modern medicine, but they are not a cure-all. To make sure they work effectively and safely, we must avoid these common myths and use antibiotics in a responsible, informed way. Here are some key takeaways:
1. Confirm the Infection Type: Antibiotics should only be used for bacterial infections, not viral infections like the common cold or flu.
2. Follow the Prescription: Always take antibiotics exactly as prescribed, without skipping doses or stopping early.
3. Don’t Self-Diagnose: Never self-prescribe antibiotics—always consult a doctor before taking them.
4. Be Aware of Side Effects: Pay attention to any side effects, and consult a doctor if anything unusual occurs.
By using antibiotics responsibly, we can not only recover more effectively but also help prevent the rise of antibiotic-resistant bacteria. Let’s work together to protect this valuable resource and ensure antibiotics continue to work when they’re truly needed!
